Donating breastmilk is probably one of the best gifts you can give to a mother and her baby. Unfortunately, milk donation is not as popular as it should be. We’ve quickly been resorting to cow/soy based formula, instead of human breastmilk. Mothers aren’t aware they can donate/receive breastmilk. They’re unsure where to donate their breastmilk, what the process entails, and even how to manage pumping and the risk of oversupply. This post will go over why you’d want to donate, where to donate, and how to donate and pump without causing an oversupply.
The benefits of breastmilk
Breastmilk saves lives. According to the World Health Organization, “breastfeeding could save more than 800,000 lives every year, the majority being children under 6 months. In addition, nearly half of all diarrheal diseases and one-third of all respiratory infections in children in low- and middle-income countries could be prevented with increased rates of breastfeeding.”
Breastmilk contains a variety of bioactive agents that modify the function of the gastrointestinal tract and the immune system, as well as in brain development, according to a study by Martin et al. It not only contains carbohydrates, protein, fat, vitamins, and minerals, but it also contains digestive enzymes, growth hormones, immune cells, and other bioactive molecules. It’s filled with human milk oligosaccharides (HMO) that have anti-infective properties that fight against pathogens. HMO’s are prebiotics, which help with baby’s probiotics, and the gut flora.
Formula on the other hand, is manufactured to replace breastmilk and is designed with the basics for proper growth and development, however it lacks the bioactive molecules, digestive enzymes, immune cells, and other “life saving” components.
When mothers donate their breastmilk, they are able to provide babies with these life saving components.

Why Donate?
There are many reasons why mothers are in need of donors milk. Some reasons are mother delivered a premature baby and her milk has not fully come in yet (being a premature baby, puts baby’s health at risk, that breastmilk can help improve.) Mother may have experienced complications at birth, that has delayed her milk from coming in, so instead of offering formula, mom can offer breastmilk. Mom’s supply may have decreased for various reasons, and instead of giving formula, mom would like to give breastmilk. Mom has an adoptive infant. Or perhaps a mother has insufficient glandular tissue (IGT), polycystic ovarian syndrome (PCOS), thyroid disorders, or even breast surgery, amongst other possible reasons.
Human breastmilk is designed for human babies. Formula, which is typically derived from cows milk or soy products, is second best to breastmilk.
Now that we know the benefits of breastmilk, and why babies would need donated milk, how can a mother go about donating milk and how can a mother who needs breastmilk, go about receiving breastmilk?

The Types of Milk Donations
There are two ways to go about donating milk. There is both informal and formal milk sharing
Formal Milk Sharing
With formal milk sharing, milk donation is handled by two types of organizations – non-profit organizations, and for profit. The non-profit organization is Human Milk Banking Association of North America (HMBANA),which uses grants and donations to operate. HMBANA currently has 28 milk banks in North America. (Check out this link to find the closest milk bank to you). The for profit organizations are Tiny Treasures Milk Bank, and Helping Hands Milk Bank used by Prolacta Bioscience, to make human milk nutritional products. They accept your donor milk, then turn it into a profit when they sell their products, which are human milk-based fortifier, and human milk caloric fortifier, for babies in the NICU.
Each bank, follows strict screening, processing, and dispensing guidelines. These guidelines were developed with the help from the Centers for Disease Control (CDC), the US Food and Drug Administration (USDA), as well as the American Academy of Pediatrics (AAP). Each bank must also abide by their specific state department of health. There is a strict standardized protocol for collecting milk and screening donors, since this milk is given to very ill or premature babies. Mothers of healthy full term babies, generally cannot obtain milk from these established milk banks or they cannot afford the cost.
In order to donate to a formal milk bank, you must go through a screening process and answer a series of health questions, as well as provide a blood test. Once approved, your milk will then be pasteurized, and tested for pathogen growth. Milk banks, go through labor intensive steps, to ensure that donor milk is safe for the most vulnerable babies. This is why donor milk through a milk bank is very expensive and are strictly used for very ill and premature babies.

Does pasteurizing breastmilk kill the immunological properties?
Many people think that pasteurization kills and significantly changes the breastmilk composition, but does it? Since milk banks are providing breastmilk to the most fragile infants that cannot afford to risk the every-day types of viruses that moms encounter, milk banks must pasteurize the milk. The things that do get killed during pasteurization, is what we want – pathogens and viruses.
The HMOs in breastmilk are retained, while partial amounts of antibodies and immunological properties also remain. Researchers are always looking for new ways of pasteurizing including ultrasonication, and high-temperature short-time to protect and preserve the benefits of breastmilk. Currently, HMBANA uses the Holder Pasteurization Method, which does impact some of the biological activity of the milk, but many of the more important compounds are either retained completely or partially.
The risk of the pathogens and viruses, far outweighs the risk of killing some of the antibodies. Babies will thrive and benefit from pasteurized breastmilk.
Informal Milk Sharing
Informal milk sharing, follows no guidelines. It involves sharing your breastmilk with sisters, neighbors, friends, and even strangers. The different health authorities, FDA, AAP, and USDA, have raised concerns regarding informal milk sharing, due to the risk of transmitted diseases and contaminants, like drugs, alcohol, and tobacco etc. This process is not regulated and it is up to your discretion.
There are several organized informal milk sharing networks that connects donors with recipients. Eats On Feets, Human Milk 4 Human Babies (HM4HB) and Only the Breast.
Typically you will connect with a mother through one of these sites or a Facebook group and you can either meet up with the mother in person, or you can ship it. You may also decide to donate your milk to a friend or family member you know and not use one of these social networks. Many moms will use informal milk sharing if their supply has decreased and instead of supplementing with formula, they supplement with donors milk, which I personally believe should be the norm.

Receiving Breastmilk
Just like informal and formal milk donations, there is also informal and formal milk recipients. If your baby is critically unstable and is in the NICU, then you will most likely receive formal donors milk (from milk banks). You also have the option of requesting milk through informal milk sharing via the websites mentioned above, Facebook groups, or word of mouth. Many cities have their own Breastfeeding support groups, where you may ask for donors milk. With everything, be cautious and it is to your own discretion.
How to pump without causing an oversupply
Now, if you’ve decided to donate your milk, but are worried about pumping and causing an oversupply, there are ways to manage this. Since the amount of milk your breasts make is all based on supply and demand, you want to be careful how often you’re telling your breasts to make milk. If you’re feeding your baby, then pumping soon after, your body will think you have twins, and it will continue to make milk for “twins.”

1. The early weeks
The first couple weeks, your breasts are still regulating and trying to figure out how much your BABY needs, so I do not recommend pumping. To start donating early on, while exclusively breastfeeding your baby, I recommend using the Haakaa or something similar to collect any dripped milk and collect that. If you do feel like you need to pump those early weeks to take the edge off of your engorgement, which note: you do not want to empty your breasts when you’re engorged, but simply pump to relieve discomfort, then you can use that pumped milk as donor milk. Your supply regulates, around 6-12 weeks, in which you won’t notice your breasts “feeling” full, and they may feel empty, however this is not the case.
2. Decide how often you’d like to pump
Let’s be real, if you don’t have to pump, why would you?… pumping is a lot of work! It sucks! So decide what you can commit to. Some moms pump just once a day, while others 2-3 or more times a day. If you know the mother, you might have more motivation to pump, than if you didn’t. Deciding how often you’re able to pump, can help with your motivation and commitment.
3. Decide when to pump
Create a Fictitious Feed
Once you’ve decided how often you want to pump, say it’s 2 times a day, then you’ll want to set 2 fictitious feeds in your day. As you start to stick to this schedule of your fictitious feeds, your body will adapt because it is expecting that milk to be removed at that particular time.
For example, I’ve decided to just pump once a day. I do it everyday around 10-11pm after my baby goes to sleep, which is 9pm. My body has adapted to produce milk at this time.
Your breasts are never empty and you could essentially pump whenever you want, however by setting a general time, this tells your body to always have milk at that time.
Pump as you feed
Another option is to pump the side that your baby is not nursing on. This will save you time from having to pump at a separate time. If your baby only takes one breast, this might be an effective way to – ‘kill two birds with one stone.’ I only recommend doing this if your baby takes one side, as you don’t want to pump, then feed your baby afterwards on that same breast, as this can eventually cause an oversupply.

4. Use hands on pumping
When you’re pumping, you want to use hands on pumping. This is when you use your hands and compress the breasts, especially once your milk flow slows down. Pumps are not able to fully drain the breast, they really only get the milk towards the front. When you compress your breast, you are accessing milk ducts far back in the breast tissue and releasing the milk.
According to a study by Stanford University, they found that mothers that hand expressed once their milk output slowed down with the pump, were able to make double the amount of milk than if they only pumped without using their hands! So if you want to save yourself time and maximize your milk output, start incorporating your hands.
5. Date and record how many ounces you pumped
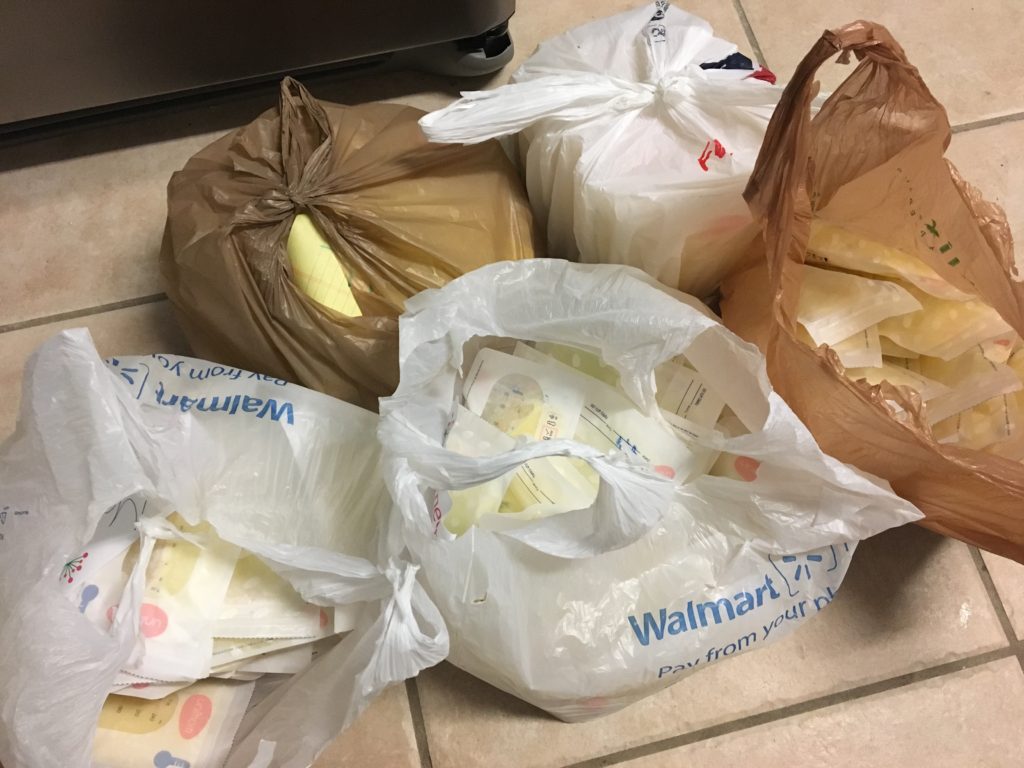
Put your breastmilk in 3-4 oz pumping bags and date it and note how many ounces it has.
6. Store in the freezer
Freeze the milk flat in the freezer, then once frozen, you can put it upright.
Depending on how you plan to donate (informal/formal), there may be different options for how to store your milk.
If you would like assistance and more guidance, please do not hesitate to contact me
In conclusion
In conclusion, it’s important to know where you’re donating your milk to – for profit, or nonprofit formal donations, or informal sharing. Giving your breastmilk is saving lives and helping to prevent illnesses.
When you give through a milk bank, you can trust you milk is going to the most compromised and vulnerable babies. These organizations are in need of more donors, to meet the demands of NICU babies in distress. However, by going through a milk bank, you won’t know who exactly your milk is going to or what city. With informal sharing, you know exactly who it’s going to, and you know what the circumstances are. It’s up to you to decide where you’d like to donate. Either way, you are doing an amazing selfless act and this is the best gift you could ever give a mom and baby.
Donors milk needs to be the norm. Human milk for human babies.
Have you been a breastmilk donor or recipient? I’d love to hear your experiences in the comments! Let’s normalize milk sharing.